Convertino selected 2013 top EMS innovator
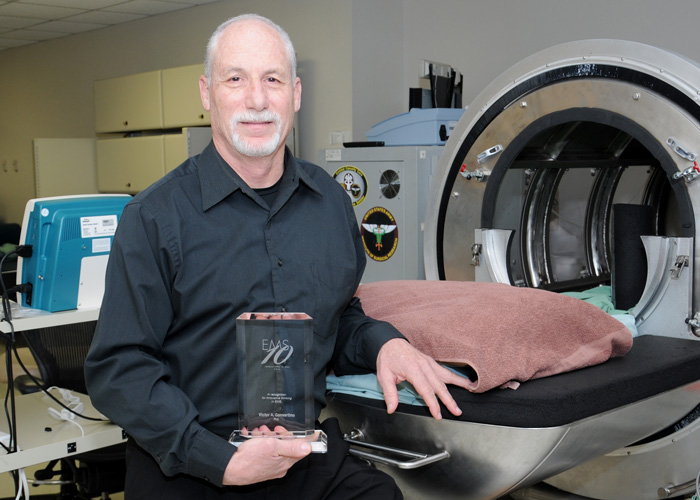
The Journal of Emergency Medical Services selected Victor A. Convertino, Ph.D., a physiologist/researcher and the tactical combat casualty care research task area program manager at the U.S. Army Institute of Surgical Research (USAISR) at Joint Base San Antonio'Fort Sam Houston, as a 2013 top innovator in emergency medical services (EMS).
Convertino was among 10 trendsetters who were recognized Feb. 5 at the 2014 EMS Today Conference and Exposition in Washington, D.C., for his efforts in developing the Compensatory Reserve Index (CRI) and the Intrathoracic Pressure Regulation (IPR) -- two life-saving technologies.
"This is a great honor that is especially significant to our research team and the U.S. Army Combat Casualty Care Research Program because it's given by a leading organization in the field of emergency medical care that is independent of the military," said Convertino. "As such, this award reflects an appreciation from our civilian counterparts that we've been successful in developing medical technologies that can be translated to any emergency medical setting to help civilian paramedics as well as our combat medics save lives during prehospital care and transport of patients."
"Vic is one of the leading prehospital researchers in San Antonio. His work is ongoing, but it is great to see one of our area's behind the scenes guy be recognized on a national level," said Dr. Craig Manifold, former director of the San Antonio Fire Department EMS.
CRI uses an algorithm designed to take information from a patient's finger pulse oximeter and gauge whether immediate medical attention is needed -- even if the patient seems alert and responsive. It is the first device of its kind that can truly detect when a patient seems stable but is actually getting dangerously worse, known as "crashing."
IPR therapy is used to create a vacuum in a patient's chest cavity to increase blood circulation and pressure. The IPR concept was used to manufacture a small breathing device called the ResQGARD that helps patients with severe low blood pressure.
"The human body has many physiological mechanisms that compensate to maintain a constant blood pressure when there's internal bleeding," explained Convertino, of the CRI. "The blood pressure can seem stable, but the patient can be losing their ability to continue to compensate. When the patient gets to the end of their compensation, their blood pressure falls rapidly, referred by some as 'falling off a cliff' and now they are in shock because we were watching their blood pressure rather than a measure of their reserve to compensate."
In order to measure a patient's reserve to compensate, Convertino focused on an arterial waveform that is created by blood going out into the vessels.
"Each time the heart pumps, a pulse of blood creates an arterial pressure wave that is actually made up of two waveforms," he said. "The first waveform, called the ejected wave, is caused by the blood leaving the heart, and the second wave called the reflected wave is caused by the blood being reflected off the arteries back to the heart. These events happen so quickly that the two pressure waves are merged so they look like a single waveform.
With newly advanced computer technologies, they now have the capability to measure features of each arterial waveform that reflect the sum of all mechanisms of compensation that affect the heart (ejected wave) and the arteries (reflected wave), according to Convertino. They call this measurement the 'compensatory' reserve.
"If you're monitoring blood pressure in a patient with internal bleeding, you may not notice the problem because the body is compensating for the blood loss," he said. "The algorithm can gauge how much the body is compensating and how much the body has left to compensate."
Originally, the algorithm was developed with the help of robotics engineers and a pediatric trauma surgeon at the University of Colorado with unique biomedical engineering talents of combining machine learning with feature extraction capabilities. These engineers used data gathered from more than 250 men and women studied in a lower body negative pressure chamber that produces responses in humans similar to those observed in someone bleeding, but without losing an ounce of blood.
Convertino and his task area began a clinical trial earlier this year on 20 human subjects to gather data for submission to the Food and Drug Administration (FDA) for 510(K) clearance. The FDA uses the 510(K) premarket submission to ensure that a medical device is safe for use on patients and can then be made commercially available.
"This is so new that we really have to demonstrate that it works," said Convertino. "No one has done this before, but we're pretty confident that we can meet FDA requirements."
Separately, IPR was created in collaboration with Advanced Circulatory Systems Inc.
"What the IPR does is provide resistance during a patient's inspiration, so that greater negative pressure is created in the thorax. That sucks more blood to the heart and brain," said Convertino. "It's so eloquently simple that I'm almost embarrassed that I didn't think of it first."
The devices that deliver IPR therapy are lightweight and easily fit in any medical or first aid kits on or off the battlefield.
IPR therapy has been used in the pre-hospital setting to assist in saving countless lives, particularly in cases of cardiac arrest, and provides rapid resuscitation without the use of fluids. As a result, the ResQGARD has been deployed in the medical kits of air and land ambulances as well as battalion aid stations on the battlefield.
"This award recognizes Vic's unwavering search for better understanding of human physiology and better ways to treat patients in emergent situations," said Dr. Keith Lurie, inventor of the IPR concept. "The cutting edge research that Vic and his team are conducting will prove critical in the advancement of capabilities for EMS care on the national level as well as on the battlefield."
 An official website of the United States government
An official website of the United States government
 ) or https:// means you've safely connected to the .mil website. Share sensitive information only on official, secure websites.
) or https:// means you've safely connected to the .mil website. Share sensitive information only on official, secure websites.


