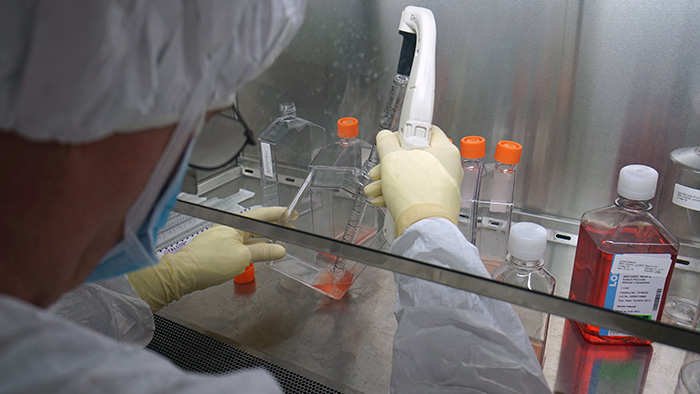
WRAIR developed, manufactured and tested the Purified Inactivated Zika Virus vaccine
Three Phase 1 human clinical trials evaluating an Army-developed Zika purified inactivated virus (ZPIV) vaccine have shown it was safe and well-tolerated in healthy adults and induced a robust immune response. Initial findings from the trials were published online today in The Lancet.
Each of the three studies included in the paper was designed to address a unique question about background immunity, vaccine dose or vaccination schedule. A fourth trial with ZPIV is still underway in Puerto Rico, where the population has natural exposure to other viruses in the same family as Zika (flaviviruses) such as dengue.
"It is imperative to develop a vaccine that prevents severe birth defects and other neurologic complications in babies caused by Zika virus infection during pregnancy," said Dr. Kayvon Modjarrad, WRAIR's Director for Emerging Infectious Diseases, the Zika program co-lead and the article's lead author. "These results give us hope that a safe and effective vaccine will be achievable."
Across the three trials, a total of 67 healthy adult volunteers (55 vaccine, 12 placebo) received two vaccine injections, four weeks apart. Researchers measured the immune response by monitoring levels of Zika virus-neutralizing antibodies in the blood. More than 90 percent of volunteers who received the vaccine developed an immune response against Zika.
"Not only is the development of a Zika vaccine a global public health priority, but it is also necessary to protect Service Members and their families," said Col. Nelson Michael, director of WRAIR's Military HIV Research Program and Zika program co-lead.
The ZPIV vaccine candidate was developed as part of the U.S. Department of Defense response to the 2015 outbreak of Zika virus in the Americas. WRAIR researchers conceived the ZPIV vaccine in February 2016 and were able to advance the candidate to a Phase 1 human trial by November of the same year.
"WRAIR has previously steered to licensure a similar vaccine for Japanese encephalitis, a flavivirus in the same family as Zika, which helped speed our vaccine development effort," said Dr. Leyi Lin, who led one of the trials at WRAIR.
In the volunteers who received the vaccine, neutralizing antibody levels peaked two weeks after they completed the 2-dose vaccine series, and exceeded the threshold established in an earlier study needed to protect monkeys against a Zika virus challenge (Science. 2016 Sep 9; 353(6304):1129-32). Researchers also found that antibodies from vaccinated volunteers protected mice from a Zika virus challenge, providing insight into how this vaccine might prevent Zika infection.
Each study included in this aggregate analysis was designed to address a unique question around ZPIV vaccination:
- WRAIR Clinical Trial Center in Silver Spring, Maryland, is assessing the impact of preexisting flavivirus immunity in volunteers who received either a licensed yellow fever or Japanese encephalitis vaccine prior to ZPIV.
- Saint Louis University (SLU) in St. Louis, Missouri, is evaluating the safety and immunogenicity of three different vaccine doses.
- Beth Israel Deaconess Medical Center (BIDMC) in Boston, Massachusetts, is evaluating three different ZPIV dosing schedules.
Next steps include evaluating how long vaccine-induced immunity lasts, and the impact of dose, schedule and background immunity. Michael added that "Army researchers are part of an integrated, strategic U.S. government effort to develop a vaccine to protect against Zika."
The ZPIV program is led by Michael and Modjarrad. The principal investigators at each of the study sites were Dr. Leyi Lin at WRAIR, Dr. Sarah L. George at SLU and Dr. Kathryn E. Stephenson at BIDMC. The sponsor of the investigational new drug application for two of the studies (WRAIR and SLU) is the National Institute of Allergy and Infectious Diseases Division of Microbiology and Infectious Diseases, part of the National Institutes of Health. The BIDMC study is investigator-sponsored (Dr. Kathryn Stephenson).
This work was supported in part by a cooperative agreement between the Henry M. Jackson Foundation for the Advancement of Military Medicine, Inc., the U.S. Departments of Defense and Army, and the National Institute of Allergy and Infectious Diseases.
One of the trials was conducted by the NIAID-supported Vaccine and Treatment Evaluation Unit at SLU (Contract # HHSN272201300021I).
 An official website of the United States government
An official website of the United States government
 ) or https:// means you've safely connected to the .mil website. Share sensitive information only on official, secure websites.
) or https:// means you've safely connected to the .mil website. Share sensitive information only on official, secure websites.